Abstract
Background:Direct oral anticoagulants (DOACs) are the new standard of care for stroke prevention in atrial fibrillation (AF) and treatment of venous thromboembolism (VTE). The consequences of concomitant use of direct oral anticoagulant (DOAC) therapy with antiplatelet therapy (APT) are less well-known compared to warfarin therapy. However, combining oral anticoagulant (OAC) with APT is known to cause an increase in major bleeding by two-fold. Recent clinical trial data and guidelines recommend that most patients on OAC should not receive APT for primary prevention of atherosclerotic cardiovascular disease (ASCVD) due to increased bleeding risk with APT. Similarly, in patients with a long-term indication for OAC and with an ASCVD event, most patients should proceed with OAC alone following at least 12 months of OAC+APT due to limited benefit and increased bleeding with combined therapy. This single-center quality improvement study aims to describe the proportion of patients on DOAC+APT and highlight potential targets for more in-depth assessment.
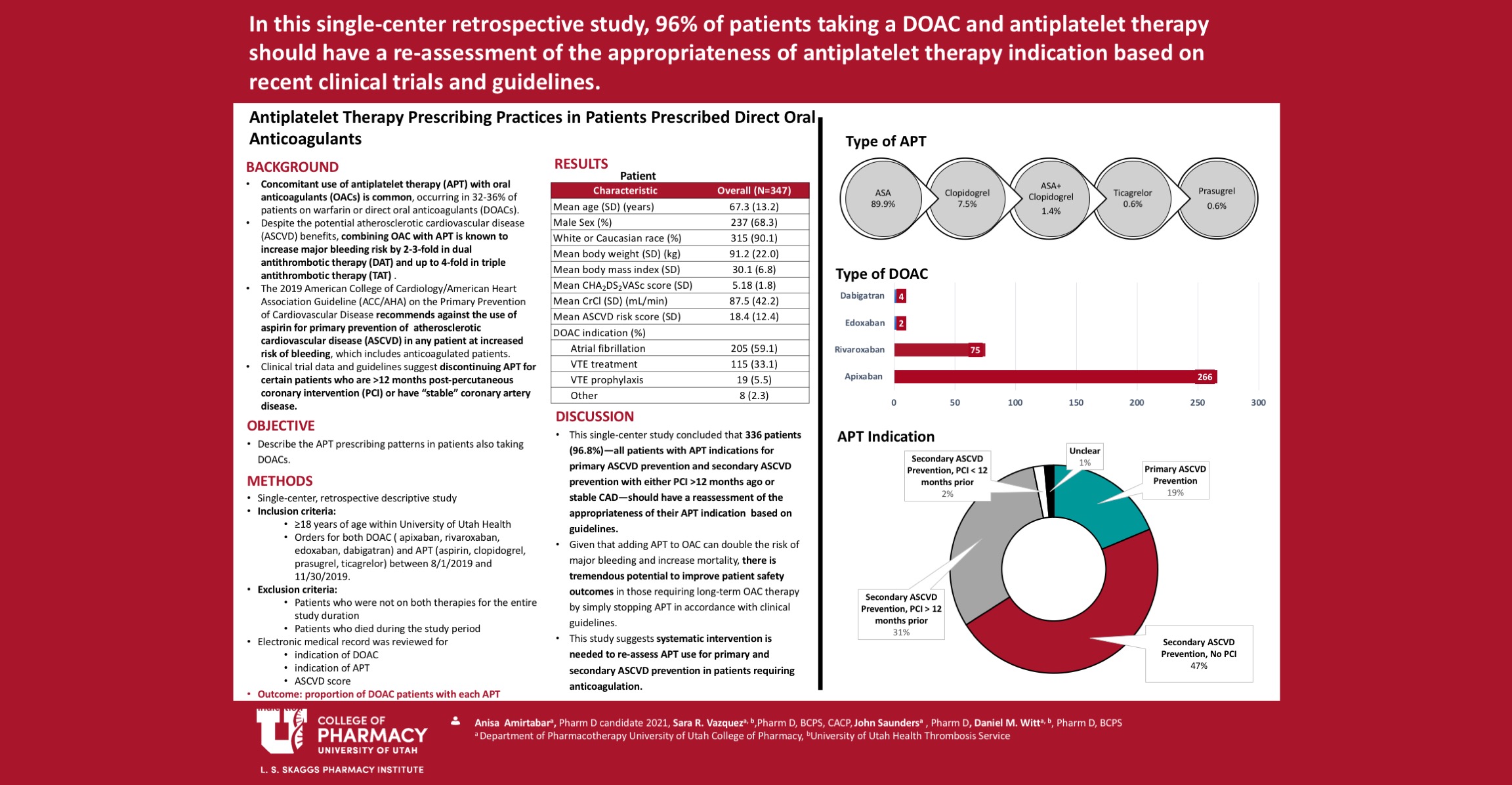
Methods: Patients within the University of Utah Health who were receiving both a DOAC and APT during a 4-month period were included. Patients were excluded if they were not receiving both therapies for the entire study duration. Included patients were categorized into four groups by indication for APT via chart review: primary ASCVD prevention, secondary ASCVD prevention with no percutaneous coronary intervention (PCI)/stent, secondary ASCVD prevention with PCI in previous 12 months, and secondary ASCVD prevention with PCI >12 months prior. The primary outcome of this study is a description of the APT indications in patients taking both DOAC and APT.
Results:During the study period, 347 patients received both a DOAC and APT. APT was combined with DOAC most commonly for secondary ASCVD prevention in patients without PCI (47.3%), followed by secondary ASCVD prevention in patients PCI > 12 months prior (30.8%), primary ASCVD prevention (18.7%), and secondary ASCVD prevention with PCI in the previous 12 months (1.7%). Five patients (1.4%) were on APT without a clear or documented indication.
Conclusions: Based on the results of this study, 96.8% of patients on DOAC+APT should have a reassessment of the appropriateness for continuing APT in combination with their OAC, based on recent guidelines steering clinicians away from using APT for primary prevention and in stable coronary artery disease in anticoagulated patients. This study highlights the tremendous potential to improve patient safety and reduce bleeding harm and can serve as the foundation for an institution-wide intervention to routinely evaluate APT use for primary and secondary ASCVD prevention
References:
- Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883-891. doi:10.1056/NEJMoa1009638.
- Agnelli G, Buller HR, Cohen A, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369(9):799-808. doi:10.1056/NEJMoa1302507.
- EINSTEIN Investigators, Bauersachs R, Berkowitz SD, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363(26):2499-2510. doi:10.1056/NEJMoa1007903
- Alexander JH, Lopes RD, Thomas L, et al. Apixaban vs. warfarin with concomitant aspirin in patients with atrial fibrillation: insights from the ARISTOTLE trial. Eur Heart J. 2014;35(4):224-232. doi:10.1093/eurheartj/eht445
- Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation [published correction appears in N Engl J Med. 2010 Nov 4;363(19):1877]. N Engl J Med. 2009;361(12):1139-1151. doi:10.1056/NEJMoa0905561
- Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093-2104. doi:10.1056/NEJMoa1310907
- Schulman S, Kearon C, Kakkar AK, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342-2352. doi:10.1056/NEJMoa0906598.
- Hokusai-VTE Investigators, Büller HR, Décousus H, et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism [published correction appears in N Engl J Med. 2014 Jan 23;370(4):390]. N Engl J Med. 2013;369(15):1406-1415. doi:10.1056/NEJMoa1306638.
- Arnett, D. K., Blumenthal, R. S., Albert, M. A., Buroker, A. B., Goldberger, Z. D., Hahn, E. J., Himmelfarb, C. D., Khera, A., Lloyd-Jones, D., McEvoy, J. W., Michos, E. D., Miedema, M. D., Muñoz, D., Smith, S. C., Jr, Virani, S. S., Williams, K. A., Sr, Yeboah, J., & Ziaeian, B. (2019). 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 140(11), e596–e646. https://doi.org/10.1161/CIR.0000000000000678
- Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42(5):373-498. doi:10.1093/eurheartj/ehaa612.
- Ortel, T. L., et al. (2020). “American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism.” Blood Adv 4(19): 4693-4738. doi:10.1182/bloodadvances.2020001830.
- McNeil JJ, Nelson MR, Woods RL, et al. Effect of Aspirin on All-Cause Mortality in the Healthy Elderly. N Engl J Med. 2018;379(16):1519-1528. doi:10.1056/NEJMoa1803955.
- Haller PM, Sulzgruber P, Kaufmann C, et al. Bleeding and ischaemic outcomes in patients treated with dual or triple antithrombotic therapy: systematic review and meta-analysis. Eur Heart J Cardiovasc Pharmacother. 2019;5(4):226-236. doi:10.1093/ehjcvp/pvz021.
- Lip GYH, Banerjee A, Boriani G, et al. Antithrombotic Therapy for Atrial Fibrillation: CHEST Guideline and Expert Panel Report. Chest. 2018;154(5):1121-1201. doi:10.1016/j.chest.2018.07.040.
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report [published correction appears in Chest. 2016 Oct;150(4):988]. Chest. 2016;149(2):315-352. doi:10.1016/j.chest.2015.11.026.
- Yasuda S, Kaikita K, Ogawa H, et al. Atrial fibrillation and ischemic events with rivaroxaban in patients with stable coronary artery disease (AFIRE): Protocol for a multicenter, prospective, randomized, open-label, parallel group study. Int J Cardiol. 2018; 265:108-112. doi: 10.1016/j.ijcard.2018.04.131.
- Kumbhani DJ, Cannon CP, Beavers CJ, et al. 2020 ACC Expert Consensus Decision Pathway for Anticoagulant and Antiplatelet Therapy in Patients With Atrial Fibrillation or Venous Thromboembolism Undergoing Percutaneous Coronary Intervention or With Atherosclerotic Cardiovascular Disease: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021;77(5):629-658. doi:10.1016/j.jacc.2020.09.011.


Responses
Anisa, this turned out really well. I like your very tightly focused aim and the results are quite provocative. What are some things that pharmacists can do to help reduce the use of combined aspirin and DOAC therapy?
Thank you so much Dr. Witt.
Definitely have an accurate medication reconciliation and verify if patient has an appropriate indication to be on aspirin are some of the ways that pharmacist can help to reduce the use of combined aspirin and DOAC therapy.
Shows all how pharmacists need to educate patients on all meds including OTC that may affect outcome.
Hey Jane,
I agree with you. Definitely, pharmacists play a huge role of making sure that patient get adequate education on their medications including OTC.
This is an important tool for pharmacists to use in the justification of continued med safety. Hope it is published soon.
Dr. Gunning,
I agreed, and I am hoping to publish soon, and waiting to see a great outcomes from it.
Great work, Anisa! I’m so proud of how hard you worked for this project and I think you have an impactful story to tell. Which APT indication do you think we should target as a priority for intervention?
Dr. Vazquez, my project would not turn great without your help. Thank you for all the feedbacks and helps you given me in the past 2 years. It was a great experience working with you, Dr. Witt ,and Dr. Saunders.
In regard to answering your question; the use of Aspirin for primary prevention or no clear indication should be the priority to target.
That would be definitely the largest area to target then modifying treatment and duration of aspirin for secondary Prevention would be the next step.
Comments are closed.