Abstract
Introduction:
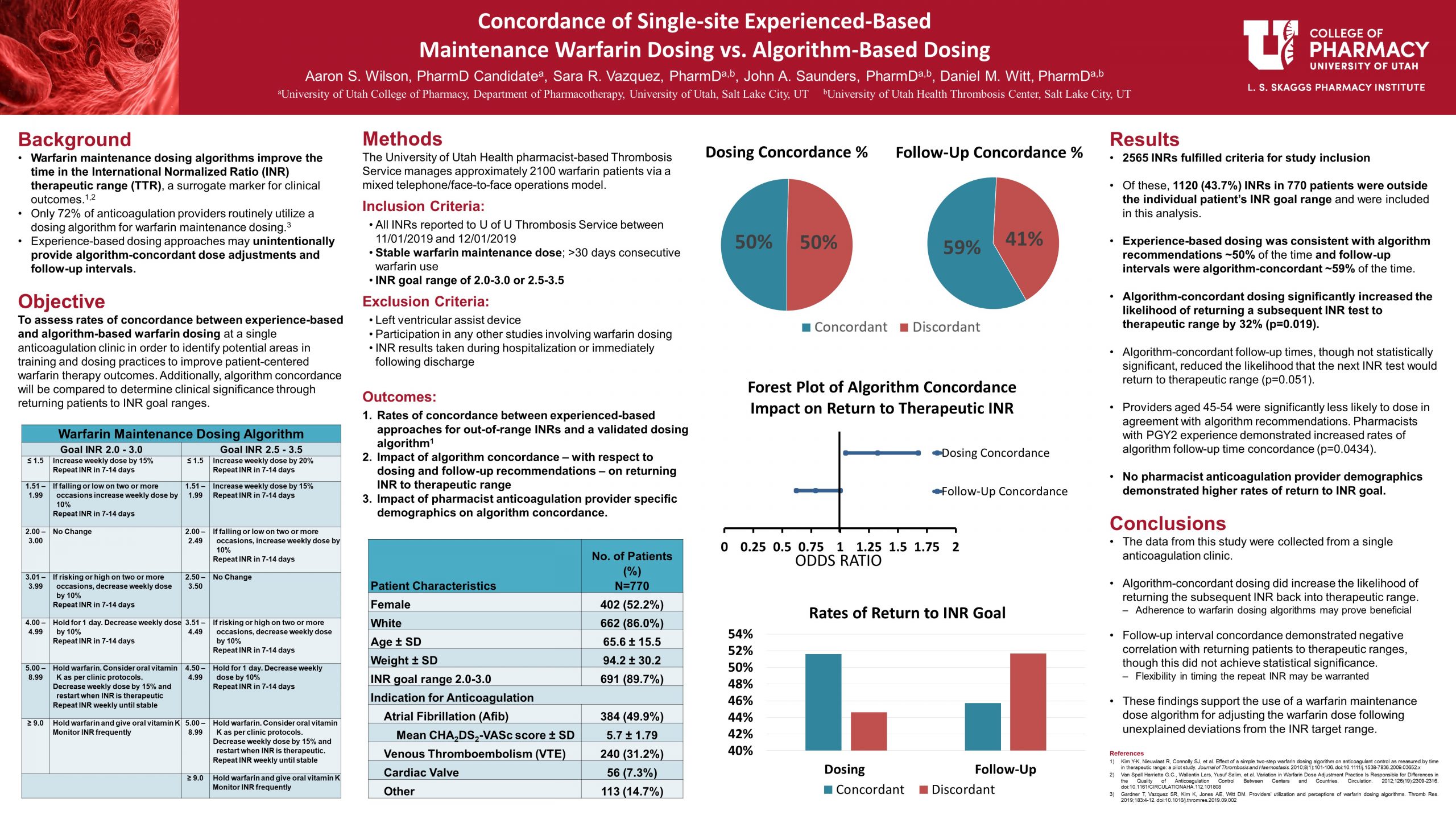
Warfarin maintenance dosing algorithms improve the time in therapeutic International Normalized Ratio (INR) range (TTR), a surrogate marker for clinical outcomes. Despite demonstrated benefits, it has been reported that just over a fourth of anticoagulation providers utilize experience-based dosing instead. This study assessed rates of concordance between experience-based and algorithm-based warfarin dosing at a single anticoagulation clinic.
Methods:
Within the University of Utah Health’s Thrombosis Service, patients in the maintenance phase of their warfarin therapy with an INR goal of 2.0-3.0 or 2.5-3.5 and who had INR results during November 2019 were included. Experienced-based approaches for out-of-range INRs were compared to a validated dosing algorithm to determine algorithm concordance rates as well as the likelihood that algorithm concordance would return the INR into therapeutic range.
Results:
During the one-month study period, there were 1120 (43.7%) out-of-range INRs in 770 patients included in this analysis. Providers’ decisions were 50.5% algorithm-concordant for dosing adjustments and 59.2% concordant for follow-up intervals. Algorithm-concordant dosing practices resulted in a significantly higher likelihood of returning the subsequent INR to the target range (odds ratio [OR] 1.325, 95% confidence interval [CI] 1.047-1.676), whereas algorithm-concordant follow-up intervals did not significantly impact return of INR to therapeutic range (OR 0.788, 95% CI 0.621-1.001). No provider characteristics significantly impacted the rate of return to INR goal.
Conclusion:
This single-center study demonstrated that experience-based dosing was 50% concordant with a validated algorithm and that algorithm-concordant dosing increased the likelihood of returning the INR to therapeutic range. These findings support strategies that either align experience-based dosing better with algorithm-based principles or strengthen the recommendation for using a validated dosing algorithm.
Key Points
- Unintentional algorithm concordance occurred approximately 50% and 60% of the time for dosing and follow-up times, respectively.
- Algorithm concordant dosing resulted in increased rates of return to therapeutic INR at subsequent INR tests.
- Follow-up time intervals did not contribute towards a significant difference in the rates of return to INR goal between algorithm concordant and discordant practices.
- Few provider demographic groups demonstrated increased unintentional algorithm concordance, though no groups demonstrated increased rates of return to INR goal at subsequent INR tests.
- Additional research of algorithm use for specific patient demographics or anticoagulation indication may prove to be beneficial in illustrating specific incidences when following warfarin dosing algorithms are optimal.
Keywords: warfarin, maintenance dosing, INR, TTR, algorithm, anticoagulation clinic
Abbreviations: Time in Therapeutic Range (TTR), International Normalized Ratio (INR)
Recommend0 recommendationsPublished in College of Pharmacy, Virtual Poster Session Spring 2021


Responses
Great work, Aaron! Poster really looks great. If you were going to design a follow up study to this project, what would it be?
Thank you for your question and for your guidance on these projects! Based upon the conclusions of this study, I would be interested to know how the benefits of using a warfarin dosing algorithm might differ between different disease states. We did not conduct a formal subgroup analysis in this study, though I believe it would provide additional insight for future algorithm use.
Additionally, the data demonstrated in this study showed non-significance in follow-up time intervals with respect to algorithm concordance. With that in mind, I would be interested in a descriptive study outlining barriers and factors that contribute to follow-up times between INR tests.
Very interesting project – i would love to see a qualitative look at what the anticoagulation providers thoughts are on algorithm based dosing and how they see themselves matching with it and why or why not. Definitely more projects could come from this area
I agree! One reference which I reviewed for this project did provide some insight into providers’ opinions about algorithm use. It was a study conducted by Trevor Gardner, a previous pharmacy student of the U. If you are interested in reading more about those results they can be found at the following address.
https://doi.org/10.1016/j.thromres.2019.09.002
Thank you. Very interesting.
Thank you for reading my poster! 🙂
Aaron, thank you for such great work! I am curious about the possible negative relation between follow-up interval and return to INR. I agree with your conclusion that perhaps strict adherence to the follow up time suggested by the algorithm isn’t necessary, but you have thoughts on why there might be this negative relation? If the follow up is discordant, does the follow-up time tend to be later, and thus might there by more time for the INR to come into range?
I am glad that you recognized the “near” negative correlation of algorithm use and return to INR with respect to follow-up time intervals! Though this did not end up being significant within our sample size, it does appear that there is something we can learn from these data.
As you have correctly hypothesized, INR retests that were later than the algorithm recommended time frame generally resulted in increased rates of return to INR goal compared to concordant follow up times, whereas shorter follow up demonstrated reduced rates of return to therapeutic INRs. I agree that time is a major factor that needs to be considered when considering the PK of warfarin and the delay in impact dose changes may have on INR.
This would make for an interested follow up study to see what factors should be accounted for when determining INR retest time frames and in what instances more aggressive monitoring practices might be recommended.
Hi Aaron! What a nice well-balanced and organized poster!! This was a great topic to investigate! I would assume that if algorithm-based dosing provided more optimal therapeutics/INR for the pts that the risk for serious adverse events would be less for pts? Good work!! Congrats, too, on the fellowship! 🙂
That is correct! Studies have shown that increasing the time that patients on warfarin are at therapeutic ranges also results in reduced rates of both bleeding and thrombotic risks. Therefore any evidence that supports returning patient to their therapeutic INR goals also contributes to reductions in these serious adverse events.
Thank you so much!!
Great poster, Aaron! We’ve already shown qualitatively that many providers don’t use algorithms for various reasons. Now that we have institution-specific quantitative data, how would you make the argument in favor of implementing algorithm use?
Thank you for all of your help and encouragement!
Based upon the results of Trevor’s project, I recognize that implementing algorithm use as a standard of practice might present opposition and other challenges. To address this, I would recommend introducing the algorithm as a before-and-after study design trial that would provide data showing longer term/more consistent algorithm use. I feel that TTR is an important surrogate endpoint that an institution might want to observe to determine the clinical significance of long term algorithm use in addition to the short term benefits demonstrated in this study. Using the combined results of these studies I feel that the argument for algorithm use would be simplified.
You did great, Aaron!
Thanks Lien! I appreciate your support!
Comments are closed.