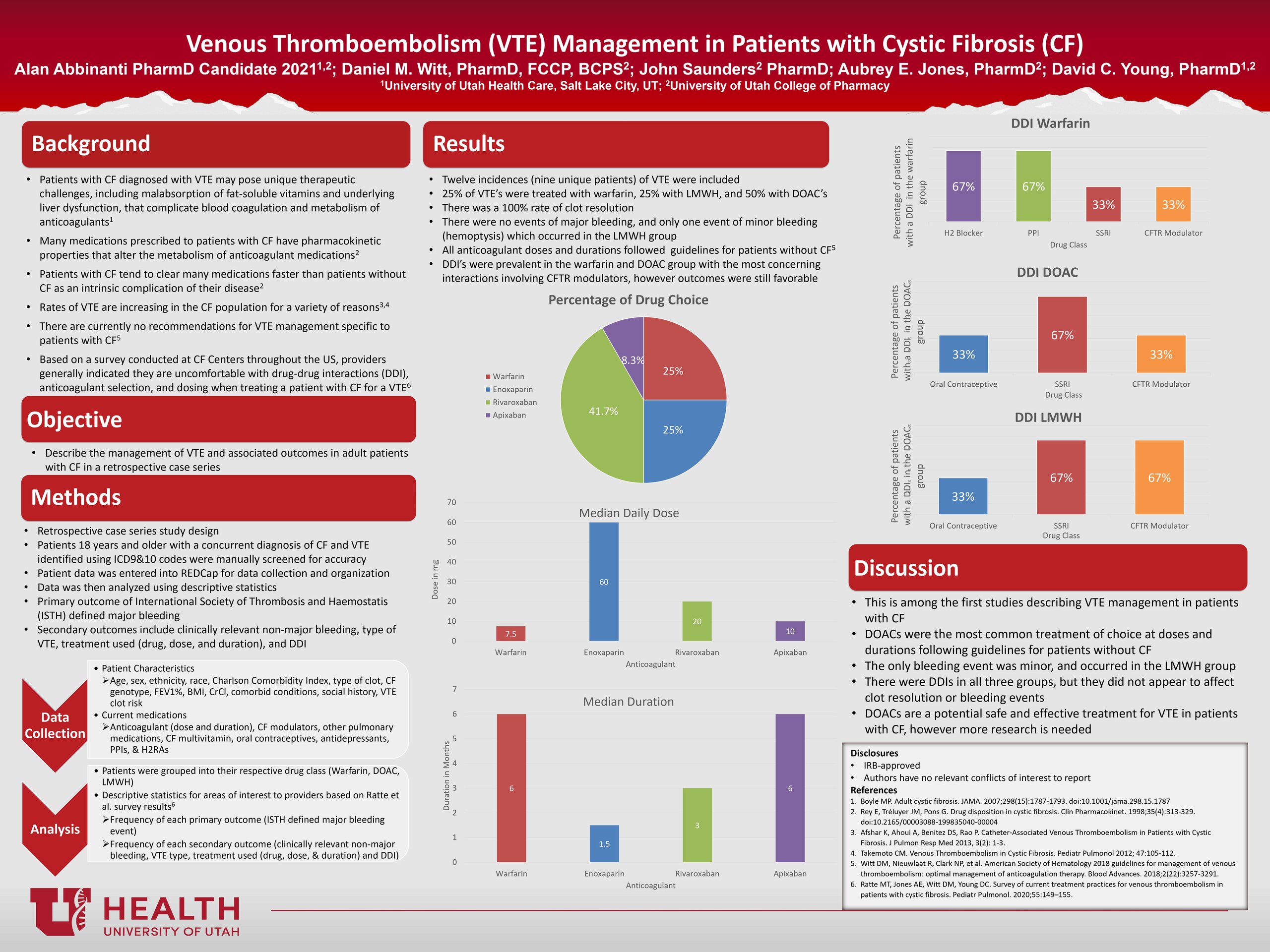
The rates of venous thromboembolism (VTE) are increasing in cystic fibrosis (CF) patients due to a variety of complications of their disease state and an increased life expectancy. A recent survey found that providers treating VTE in CF patients reported low confidence concerning drug selection, dose, duration, and drug-drug interactions (DDI). There are currently no published reports regarding management of VTE in patients with CF. An electronic medical record search was done in the University of Utah Health’s system for patients with CF and VTE. Patients were categorized into one of three treatment groups (warfarin, direct oral anticoagulant (DOAC), and Low Molecular Weight Heparin (LMWH)). The primary outcome was the International Society of Thrombosis and Haemostatis’ definition of major bleeding. Secondary outcomes included clinically relevant non-major bleeding, type of VTE, treatment used (drug, dose, and duration), and DDI. Nine patients with a total of twelve unique VTE cases were included in the study. Of the twelve VTE cases, 25% were treated with warfarin, 50% with a DOAC, and 25% with LMWH. There were no events of major bleeding and only one event of clinically relevant non-major bleeding (hemoptysis) which occurred in the LMWH group. All anticoagulant doses and durations generally followed guidelines for patients without CF. DOACs were the most common VTE treatment, at doses and duration following guidelines for patients without CF, with no events of major or clinically relevant non-major bleeding. DOACs are a potential safe and effective treatment for VTE CF patients, but more research is needed.
Recommend0 recommendationsPublished in College of Pharmacy, Virtual Poster Session Spring 2021


Responses
I think the median daily dose and median duration charts could have been tables. That would’ve saved room on your poster and allowed some of the font to be bigger so we could read it a little better. Overall, interesting study!
Thank you for the suggestion. I will consider that for future research posters that I create. I am glad you found the study interesting as well.
Nice work, Alan! Given that so many of these DVTs were associated with PICC lines, what recommendations do you have for clinicians caring for patients with CF during pulmonary exacerbations? Should they be receiving VTE prophylaxis therapy? Were there any factors that seemed to be associated with risk of DVT that might identify patients that should be carefully monitored?
Those are excellent questions. Given that we only had 12 cases of VTE that we were able to evaluate, I am not confident in making any recommendations for prophylaxis therapy. There is a need for a more extensive study of VTE in patients with CF before any recommendations could be made for prophylaxis or treatment therapies.
However, as you eluded to in your second question, patients with PICC lines should be more closely monitored for VTE as that was the most significant risk factor observed. Again, with our low numbers, we could not identify other risk factors for VTE, and a larger study is needed to identify those risk factors.
Hopefully, this study will start a conversation in the CF community regarding VTE treatment and answer some of those questions more concretely.
Thank you for your research.
Alan – interesting therapeutic issue in CF. I was unaware of this as an emerging issue. Thank you for bring this to light. What 2 things did you learn from doing this project?
Awesome work, Alan!
Comments are closed.