Abstract
Background: Gabapentin is a drug initially approved as a seizure drug but is now used for many off-label indications. The prescribing of gabapentin has grown exponentially in recent years, and much of it has been driven by off-label prescribing. With gabapentin prescription numbers rising, many are concerned that gabapentin lacks effectiveness and safety for many off-label uses.
Objective: The objective of this study is to evaluate off-label gabapentin prescribing at a family medicine clinic, compare off-label indications found to the current literature of effectiveness, and improve gabapentin prescribing quality and safety at our family medicine clinic.
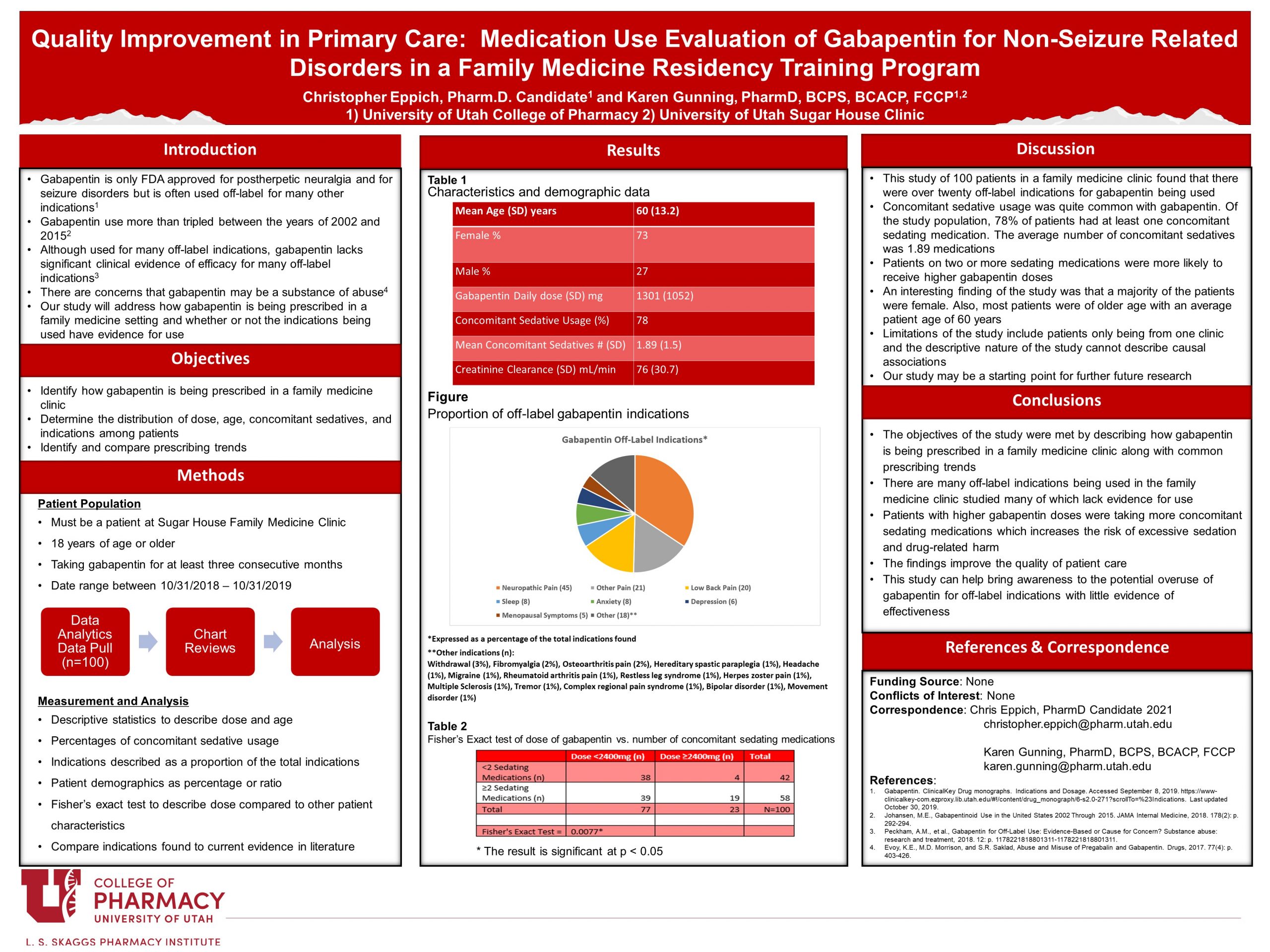
Methods: A retrospective chart review of 100 patients taking gabapentin at the University of Utah Sugar House Family Medicine Clinic was performed. Patients were randomly selected, and patient charts via electronic health records were reviewed manually. Patients taking gabapentin for an off-label indication for at least three consecutive months and who were at least 18 years of age were included. Data collected included demographics, indication for use, concomitant sedating medications, and the total daily dose of gabapentin. Descriptive statistics were used to describe data along with a Fisher’s Exact test to analyze age vs. gabapentin dose and gabapentin dose vs. the number of concomitant sedating medications.
Results: In total, 100 patients were included in the study. The study population was mostly white/Caucasian (81%) and female (73%). The average age was 60 years (SD 13.2). The mean gabapentin dose for the study population was 1301mg (SD 1052mg). Seventy-eight percent (78%) of patients were taking a concomitant sedating medication along with their gabapentin. The average number of concomitant sedating medications was 1.89 (SD 1.5). The average creatinine clearance for the study population was 76 mL/min (SD 30.7 mL/min). A total of twenty-one unique indications for gabapentin were identified for the study population. The top five indications found were neuropathic pain (45%), other pain (21%), lower back pain (20%), sleep (8%), and anxiety (8%). Only neuropathic pain, hot flashes, restless leg syndrome, and anxiety were found to have strong evidence for effectiveness in current literature. A Fisher’s Exact test performed on age (≥50 and <50 years) vs. gabapentin daily dose (≥2400mg and <2400mg) showed a Fisher’s exact test statistic value of 0.2457 (p-value <0.05). A Fisher’s Exact test performed on gabapentin daily dose (≥2400mg and <2400mg) vs. the number of concomitant sedating medications (≥2 medications and <2 medications) showed a Fisher’s exact test statistic value of 0.0077 (p-value <0.05).
Conclusion: In this single clinic, retrospective chart review of patients prescribed off-label gabapentin; there were twenty-one off-label indications for gabapentin found. Many of the off-label indications found in the study lacked significant evidence for effectiveness. Also, patients were found to frequently be taking concomitant sedating medications with gabapentin. There was a statistically significant correlation between two or more concomitant sedating medications and daily doses of gabapentin equal to or exceeding 2,400mg, showing that patients with more sedating concomitant medications are using higher doses of gabapentin. The results of this study show prescribing trends at one family medicine practice setting and can be used to improve the quality of patient care by enhancing safety and evidence-based medicine.
Recommend0 recommendationsPublished in College of Pharmacy, Virtual Poster Session Spring 2021

Responses
You mentioned that Gabapentin might be a substance of abuse. Do have any thoughts about how to figure out if that is an issue at the clinic? Thanks!
Thank you very much for your question, Dr. Henchey. This is a great question! There are many ways to tell if a patient is abusing, misusing, or diverting prescription medications. From my research and experience, identifying patients that consistently ask for early refills, consistently requesting increasing doses, dismissing non-gabapentin treatments, and filling with multiple doctors are good ways to tell if a patient is abusing, misusing, or diverting gabapentin. Gabapentin was recently added as a medication that is tracked by the Prescription Drug Monitoring Program (PDMP), so any provider with access to the PDMP can see if a patient has been getting gabapentin prescriptions from multiple doctors and when they are filling the prescriptions. I have even seen some opinion articles that state that they feel gabapentin should be tested for via urine drug screening similar to how opioids are monitored in the clinic. However, currently, urine drug screening is not common for gabapentin and I have never personally seen it performed. Monitoring for prescription abuse, misuse, and diversion can be quite difficult, so a thorough evaluation and patient assessment are needed. You also never want to assume a patient is abusing, misusing, or diverting a medication, so an open and honest conversation with the patient is highly important.
Wow, 21 different off-label indications! I’m wondering about the data (or lack thereof) you found to support these off-label uses. Which off-label indications would you feel more comfortable with based on the data you found and which would you not recommend gabapentin use?
Great project and fascinating results Chris!
Thank you for your question, Dr. Raber! The most common indication we found in this study, which is also the most studied indication, is neuropathic pain. For many people, it can be quite surprising that neuropathic pain is an off-label indication for gabapentin since it is used for this indication so commonly. However, gabapentin is truly only prescribed for post-herpetic neuralgia neuropathic pain rather than for other types of neuropathic pain such as diabetic neuropathy. That being said, gabapentin does have good evidence of effectiveness for multiple types of neuropathic pain, so I would feel comfortable prescribing a patient gabapentin for neuropathic pain. There is even a 2017 Cochrane Systematic Review on gabapentin for neuropathic pain which showed good efficacy. Some other indications that I found to have sufficient evidence of effectiveness were the treatment of hot flashes and restless leg syndrome. Some common indications for gabapentin that I would not recommend based on my research would be chronic lower back pain, headache, migraine, and bipolar disorder. Some of the other indications that I found during this study had low-quality evidence, so I am hoping that future studies will determine if gabapentin is effective for some of the other indications.
Rather shocking that drugs are used for unapproved treatment. Thanks.
Thank you for your comment, Jane! I very much appreciate you viewing my poster today. Hopefully, future studies will show that gabapentin is effective and safe for the treatment of many of the conditions we currently use gabapentin off-label for.
Hi Chris! I was curious, for the patients with concomitant sedating medications, did they generally have the same prescribers as for their gabapentin? or was it multiple prescribers? did you perhaps look to see if some of these patients were also on stimulating meds? I was always interested to talk to patients who were on like adderall and ambien together…
Great job and thanks for sharing!!
Hello Karen, thank you very much for your great question! Unfortunately, the prescriber for each of the concomitant sedating medications was not directly recorded for the study. For inclusion in the study, the gabapentin prescriptions had to have been prescribed by a provider at the Sugar House Clinic, but the concomitant sedating medications did not have that same inclusion criterion. The concomitant sedating medications were pulled from the patient’s medication list. Solely based on my recollection from doing chart reviews, a majority of the time the concomitant sedating medication was prescribed by the same provider as the gabapentin. In hindsight, I think that evaluating the prescriber for each concomitant sedating medication would have been valuable. Also, we did not evaluate for any concomitant stimulating medication. Since both stimulating medications and gabapentin both have the potential for abuse, it may have been an interesting data point to measure. What we were mainly evaluating with measuring the concomitant sedating medications was the potential for oversedation.
Thank you for viewing my poster and leaving a question!
nicely done my mentee! I think Dr Henchy’s question is a good one – I have no idea how we would do this in clinic. It’s pretty subjective – i.e. pts asking for high doses. One could use the CSD to see early fills – but I think that process is pretty hard (to get access to csd for research) – would love to see. Remember when we were worried if we would get 100 patients ??? no concern there!
Dr. Henchey’s question is a very good one! I agree, it would be a very difficult thing to measure. You could evaluate certain measures such as the number of early refill requests or the number of doctors prescribing gabapentin, but that does not give you the full picture as to whether or not the patient is abusing, misusing, or diverting gabapentin.
There was definitely no concern with the number of patients in this study! We found nearly 600 unique patients within the allotted one-year time frame. It would be interesting to expand this study to more patients and make further evaluations.
Thank you for viewing my poster and participating in the discussion, Dr. Gunning! I could not have done this study without you and your mentorship.
Comments are closed.